Advertisement
3 Myths About Genital Herpes That Get In The Way Of A Healthy Sex Life

We’ve all got our own hangups and insecurities when it comes to sex and intimacy—we’re only human. But for anyone living with a sexually transmitted infection like genital herpes, the inner dialogue can be deafening.
The fact is, literally hundreds of millions of women around the world live with genital herpes According to the Centers for Disease Control and Prevention, more than 1 in 6 women between the ages of 14 and 49 have the STI, which is to say you’re far from alone.
But it’s also important to realize that genital herpes, while a lifelong virus, is actually a highly manageable one—and it certainly shouldn’t stop you from having a fulfilling sex life.
So with help from obstetrician gynecologist Dr. Jessica Shepherd, MD and Alexandra Harbushka, a new mom who’s living with genital herpes, we’re breaking down three of the biggest misconceptions about herpes and how it impacts our sexual wellness, from both a clinical and first-hand perspective.

Myth #1. “I have to settle now.”
It’s natural that the news of getting genital herpes can come as a shock, sending you into a tailspin. “When I was diagnosed,” says Harbushka, “I immediately believed that all my hopes, goals, and dreams of marrying the person I wanted, having a happy marriage, and having children were all out the door,” she says. “I thought, do I only have sex with people who have herpes now? Do I have to settle because of this?”
The fear of rejection from a current or future partner is very real, but along the way, it empowered Harbushka to evaluate what kind of intimate relationships she wanted in her life, and also build up her own self-respect and self-love.
She explains it like this: “After a diagnosis, we tend to put our partner on a pedestal because we’re filled with guilt, shame, resentment, and embarrassment. Society has told us that if we have herpes, we’re a bad person, we’re dirty, or we’re irresponsibly having sex. That’s not true at all! So, I had to really know myself, establish my own boundaries, and get comfortable with having uncomfortable conversations,” she says. “Frankly, it’s the questions we should all already be asking each other to practice safe sex: Are we monogamous, or are we dating other people? Are you using a condom with other people? Are you asking them to get tested? Have you gotten tested?”
That confidence in the face of uncomfortable conversations about your sexual health “starts from within,” she says. Then it becomes much easier to talk about it: “Telling a partner that I have herpes does not mean that I’m telling them I deserve less. It actually means I’m standing up for myself, I’m protecting myself, I love myself, and I’m only going to expect that from you.”
And for the record, no—genital herpes doesn’t affect your fertility (though some STIs do). “I’ve had so many patients who feel as if their ability to conceive or have a healthy baby after a diagnosis is shattered, but these are big misconceptions,” says Dr. Shepherd. “You can absolutely manage any outbreak that might happen in pregnancy or close to a delivery and make sure that it’s not transmitted to your baby.”
Myth #2. “Outbreaks will end my sex life.”
“One of the reasons women feel so defeated when they’re diagnosed is they think it’s going to severely impact their sexual life and their relationships,” says Dr. Shepherd.
“That’s actually far from true.” While you shouldn’t have intercourse during an outbreak, as you risk transmitting the virus, you can find creative ways to be intimate during these times, and your relationship can still thrive.
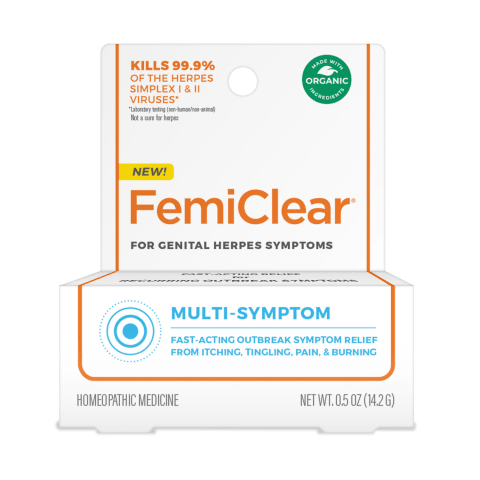
The latest advances in herpes treatments can help you lessen the frequency of your outbreaks as well as their duration, which means safe sex and a lower chance of transmitting the virus. One example of recent developments include a new over-the-counter product, FemiClear for Genital Herpes Symptoms. “FemiClear provides a really great option for women looking to manage their outbreak symptoms using all natural and organic ingredients,” says Dr. Shepherd, who encourages women to have honest conversations with their healthcare provider to figure out the best course of treatment. In vitro laboratory testing shows FemiClear kills 99.9% of the herpes simplex I and II viruses. It’s also been shown in studies to reduce the itching, pain and burning symptoms associated with genital herpes outbreaks in over 90% of women who tried it. It’s available at CVS in the personal intimacy aisle or online at CVS.com, Target.com, or Amazon.com, and designed to be used in tandem with your prescribed antiviral medication. You can use it at the first sign of an outbreak, which is a good thing, because in Harbushka’s experience, “the sooner you can get your treatments going, the sooner you can potentially prevent an outbreak from happening or lessen it to just a few days as opposed to a week.” For Harbushka, the start of an outbreak feels like a tingle—almost like a bug is walking on her skin.
At this point, Harbushka says, “Sex with my husband is normal and totally healthy. Yes, there are times when I can’t have sex because I have an outbreak—it happens. But there are times when I can’t have sex because I’m on my period and I don’t feel like it, or I’m stressed out at work, or my husband is out of town, or I’m tired. It’s just totally normal.”

Myth #3. “I have to use condoms for the rest of my life.”
First of all, it’s important to understand that condoms can’t completely protect you or your partner from HSV-2 simply because condoms don’t cover everywhere the virus is present.
That said, this will ultimately come down to what you and your partner agree is safe for both of you together. “Sex is a big deal,” says Harbushka. “It doesn’t mean that you can’t have casual sex, but you need to have conversations beforehand and a mutual understanding of what could happen.”
“Understanding how each of you define what safe sex is and how to have it will allow you to move forward into having a healthy, normal, beautiful sex life,” she continues. “So yes, you can get to a point in your relationship when you’re not going to use a condom anymore—you just need to be on the same page with your partner.”
Dr. Shepherd sees a number of patients who are in discordant relationships, meaning one person is a carrier of the virus, and the other isn’t. For them, “communication and transparency is very important. And the person who is a carrier needs to know their body really well to know when they’re about to have an outbreak so they can tell their partner.”
That’s exactly how Harbushka handles it with her husband. “I’ll say, ‘OK, something feels off,’ and he’ll say, ‘no problem.’ And instead of having sex, we’ll get creative and do other things—or not. The important thing is that having herpes isn’t a one-time conversation—this is a conversation that has to be so normal that it can come up over dinner. ‘I feel an outbreak coming on’ needs to be as natural as ‘I hit my funny bone today, and it really hurt!’ Talking about it with your partner needs to go from being uncomfortable to a normal, everyday exchange.”
The bottom line? The more you know and understand about genital herpes, the less about it you have to fear and the sooner you can return to the fulfilling sex life you’ve been missing.